Future-Proofing Medical Schools With Flexible, Adaptive Design
- By Randy Kray, Ami Shah
- 03/01/19

IMAGE COURTESY OF HOK
Health care policy and patient care delivery methods have seen significant evolution with the advent of electronic medical records, artificial intelligence (AI), telemedicine, and other new technologies and methodologies. The impact of IoT and big data and the exponential increase in complexity and vastness of medical information have made it impossible for one physician or health care provider to know all aspects of care. Instead, large teams of specialized care givers are now involved in administering care for a patient.
New Learning in Older Spaces
In order to adequately prepare learners for the changing and complex world of health care, medical schools are adapting new pedagogies that emphasize experiential and interprofessional education. Specifically, medical schools are shifting from a learning philosophy rooted in rote memorization to one that prioritizes self-motivated, just-in-time learning coupled with a foundational knowledge of basic and clinical sciences. Problem- and team-based learning play a major function in this new approach to medical education.
Schools now face the challenge of trying to shoehorn modern curricula into traditional medical school environments such as lecture halls, formaldehyde-emitting dissecting rooms, and other static learning spaces from the past. This issue is particularly apparent within testing and evaluation spaces.
When it comes to testing, the identification of competencies, determination of performance levels, and assessment can happen only in spaces that allow for impediment-free, direct observation and feedback via optimal cameras, microphones, and other AV capabilities. These environments serve an important role in medical training, but they also run the risk of being over- or underutilized, depending on lesson plans and evaluation schedules. When built as static environments, these costly and high-tech spaces also can become quickly outdated given the speed in which medicine and technology are changing.
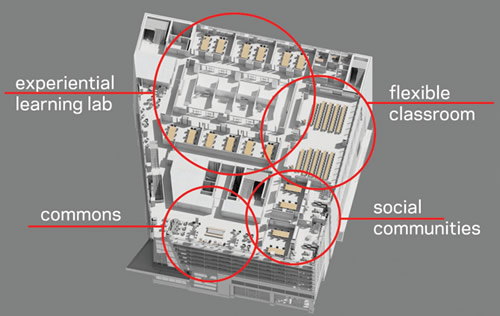
IMAGE COURTESY OF HOK
Evolving Environments
In contrast, formative practice environments need not be confined by the need for such demanding technology and space constraints and should be able to adapt to the needs of different learners both during and after scheduled training hours. New flexible, interactive spaces bridge the divide between didactic theoretical learning and experiential, immersive learning modalities. These spaces need to be able to respond to conflicting demands and priorities between teaching and testing, large group and team-based instruction, and be hyper-flexible across all these education approaches.
University of South Florida’s (USF) Morsani College of Medicine and Heart Institute, a 320,000-square-foot facility now under construction in downtown Tampa, was designed to address evolving needs of today’s medical and health educator. The new facility benefits from USF Health’s nearby Center for Advanced Learning and Simulation (CAMLS) that provides the infrastructure for training, testing, and evaluation for both undergraduate and graduate medical students. This allowed the Morsani College of Medicine to focus on other advanced models for undergraduate learning. The outcome is a hyper-flexible ecosystem of learning and support environments that work in multiple ways to build foundational and integrated health science and clinical science learning, develop team skills, and enhance the wellness of the whole person.
The centerpiece of the new learning environment at Morsani is the Experiential Learning Laboratory (ELL). Designed like a black-box theater, this immersive environment features movable, whiteboard panel walls and theatrical grid ceilings that allow the learning environment to flex to support a host of instructional needs including didactic, small-group, hands-on, physical demonstration and exam preparation. This flexibility also can be used to create round-robin workstations, enabling students to move quickly from one station to another. The intentionally “low-tech” design of these spaces means they are not beholden to any single type of teaching tool or hardware but instead can always accommodate the latest simulation technology.

IMAGE COURTESY OF HOK
Elsewhere throughout Morsani, the school’s multimodal approach to learning cycles students through spaces designed to push learning and experimentation with the ultimate goal of creating integrated thinkers. Flexible classrooms easily pivot from lecture to group-study spaces to large format interprofessional education sessions. Social communities and common areas offer students areas for individual study and rejuvenation (breakrooms, showers, lounges) after class or a long day of evaluations.
Inherent in all these design approaches is flexibility—the flexibility to address the following needs:
- The ever-changing nature of health care and the technology that supports it.
- Evolving methodologies for medical learning, from didactic instruction to experiential and interprofessional education.
- The changing ways students choose how and when to study.
- Maximizing the efficiency and use of facility space.
Tomorrow’s medical schools, faculty, and students may have an even greater list of needs than these. But that’s not a problem, provided the spaces we’re designing today have the flexibility to accommodate evolving requirements.
About the Authors
Randy Kray, AIA, OAA, MAA, is HOK's director of Science + Technology and has planned and designed advanced lab and technology facilities for clients around the world.
Ami Shah is a senior lab planner who specializes in university science and medical facilities.